

Elevated Temperature Screening | Shop Instruments | Consulting Services | Elevated Body Temperature FAQs | Elevated Body Temperature White Paper
Elevated Body Temperature (EBT) Scanning in the Time of COVID-19
White Paper by Howard Zion, Director of Service Application Engineering
The New Reality
The world is forever changed. Every country, every town, every person. And it does not matter whether you believe COVID-19 is real. The end result is the new reality that we must all face. This new reality requires us to take greater precautions than we did prior to COVID-19. If we are going to get the world economy back into motion before individual country economies collapse, we will have no choice but to put safeguards into place. It’s not just the non-believers who throw caution to the wind that are driving it, though that in itself is at the top of the list during a pandemic. But even for those taking precautions, there is still unintentional transfer occurring which provides a route for the virus to spread.
100% isolation for a period of 14 days or more is one way to stop this infectious disease. But unless you can control all 7.6 billion humans and countless more animals on the planet to be compliant with a world-wide quarantine (Venetian: quarantena meaning ‘forty days’ related to the Black Death plague in the 14th century), that is simply not a realistic solution. We can’t stop taking care of the sick or the elderly. We can’t stop taking care of our babies, children or pets. We have to go on living, but we must do it in a way that significantly minimizes transmission of infectious diseases. We must do it in a responsible manner that allows us to continue to live and work and travel and interact with each other. In the United States, the Centers for Disease Control and Prevention (CDC) as well as the World Health Organization (WHO) with a focus on international public health have developed guidelines we can all easily adopt as responsible human beings. Many countries, companies, and individuals have already implemented these safety measures. That’s a step in the right direction, erring on the side of caution.


What other steps can we take to further reduce transmission of pathogens besides isolation, cleanliness, and the use of Personal Protective Equipment (PPE)? Some businesses are checking the temperature of people who enter their facility as well as asking a short series of questions designed to identify those that might be at a higher risk of transmitting the disease, even unwittingly. But that method increases risk to the employee(s) performing the monitoring process… and then there is the cost of the employee(s) whose full-time job is to monitor people! This represents a new cost to each business which decreases the company’s profit margin or possibly increases their prices, or a combination of the two.
And what if your business requires monitoring of multiple people at once? Grocery stores, banks, restaurants, airports, et.al. need a more efficient solution to identify and mitigate health risks than to monitor one person at a time. If your business has peak periods of traffic flow, both for employees coming to and leaving work and for clients and suppliers visiting your facility, you also need a more efficient solution. That solution is infrared (IR) detection using a thermal imager or a line scanner. For many years these instruments have been used in many applications from predicting when an electric motor is about to fail to spotting heat loss around windows and doors in your home (see fig. 1). But they can also be used to detect Elevated Body Temperature (EBT). There are a few things you need to know before you buy an IR thermometer (commonly referred to as a non-contact thermometer) or a thermal imager or a line scanner for that matter.
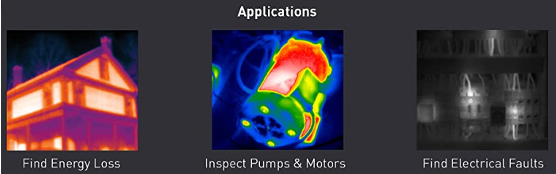
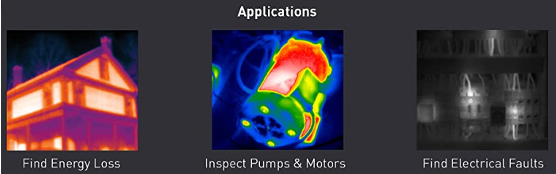
Figure 1: Applications for Infrared technology
So Many Choices, So Little Time!
For the purpose of detecting EBT, the target temperature range is 37 °C (98.6 °F) with an upper range of 38 °C (100.4 °F), identified by the CDC as the level of a fever that requires isolation. The instrument you choose for these measurements must be accurate enough to give you a correct reading. There are many non-contact thermometers available on the market. Some have an accuracy of ±0.3 °C (±0.5 °F) while others are as wide as ±2 °C (±3.5 °F). With this latter example, if you’re not paying attention to the accuracy, you could get a reading of 98.6 °F and, due to the inaccuracy of the instrument, the true temperature could be as high as 98.6 °F + 3.5 °F = 102.1 °F! In that situation, the person being monitored would likely exhibit other symptoms; the point being that you are not getting valid measurements because you’re not using the right tool for the job. In the case of the more accurate non-contact thermometer, a reading of 98.6 °F might be as low as 98.6 °F – 0.5 °F = 98.1 °F or could be as high as 98.6 °F + 0.5 °F = 99.1 °F. A much more acceptable level of confidence, wouldn’t you agree?
Why Calibrate?
What happens when the measurement of an individual is 100.0 °F? Taking the inherent error of the instrument into account, the temperature could actually be 100.0 °F + 0.5 °F = 100.5 °F. And that holds true as long as the instrument has maintained its expected accuracy, according to the manufacturer of the thermometer. Instruments change value over time due to many factors, including aging of the electronic components, handling and care of the instrument, environmental effects, etc. How do you make sure the instrument continues to read correctly? That is the reason to have the thermometer calibrated on a recurring basis. A calibration laboratory has the means to compare your thermometer against more accurate instruments in a controlled environment in order to determine the amount of error in your thermometer. If the error exceeds the manufacturer’s stated accuracy, the lab will not only make adjustments to the instrument to restore the correct readings but will also report the error to you on a calibration report, which you can then review against the temperatures you have taken to determine if the outcome would have resulted in anyone having an EBT at or above the CDC threshold of 100.4 °F. That measurement on the day the person was checked would then be called a ‘False Negative’ because it was thought at the time that the person did not have a fever when they really did have one. This is also why it is important to have a Contact Traceability list: so that anyone exposed to this person can be contacted/alerted to potential COVID-19 risk without revealing the person’s identity (following HIPAA laws). I realize this sounds like a lot of work and perhaps you aren’t maintaining a Contact Traceability list… yet. I defer to the previous statement about unintentional transmission. Infectious disease doesn’t care if we are diligent or lazy about eliminating every path/route; if we give it an inch, it will take a mile!
Thermal Imagers and Line Scanners
In order to efficiently monitor the temperature of multiple people at once, a non-contact thermometer will not do. This is where Thermal Imagers and Line Scanners provide a solution, such as the Fotric 226B or Ametek Land Viralert3, available at Transcat.com. This method of monitoring typically requires a queue to be formed, which can be as simple as selecting a hallway that naturally confines people to a defined area as they are passing through, or may require barriers to form a defined space where the monitoring will occur. These instruments usually have wider accuracies than do thermometers. So, while they are more efficient for monitoring larger masses of people, they are not always as accurate as a thermometer. That is where the concept of relative measurement vs absolute measurement becomes important to understand. If you want to know the exact temperature of each individual passing through the queue, this is not the method to use. But, if you want to detect the individuals who are running hotter than the others passing through the queue, this use of technology is brilliant! The relative temperature of individuals who have a fever will show on the imager/scanner as a different color than those whose temperature is normal. Those few potentially febrile individuals can then be pulled aside for a secondary, more accurate temperature check using a thermometer.
Calibration of Thermal Imagers and Line Scanners
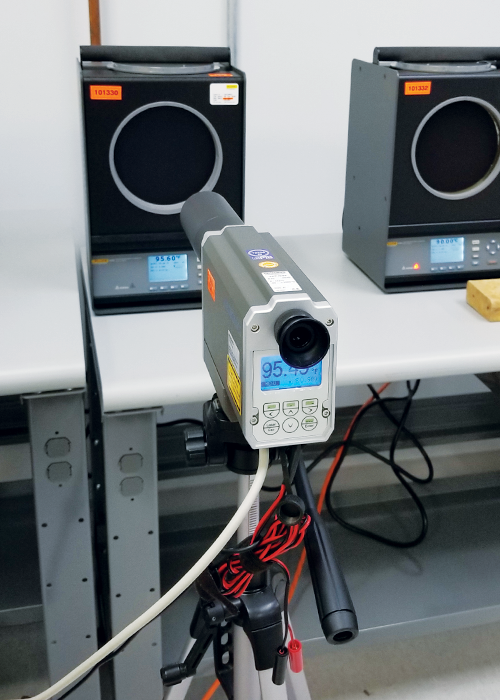
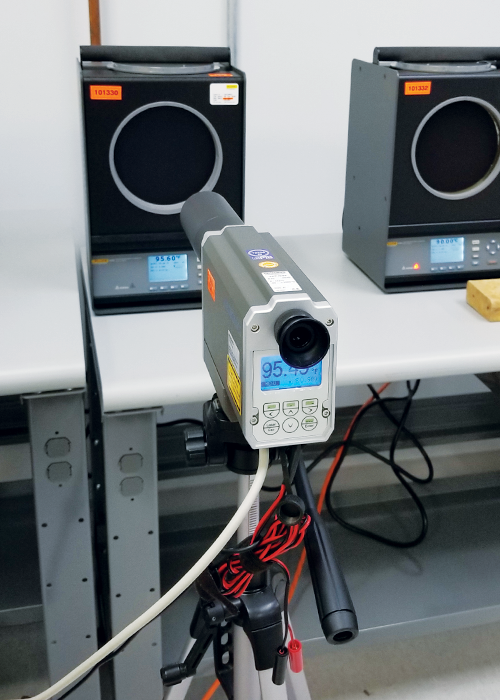
The calibration of these instruments is still very important because, even for relative measurements, you need to ensure the difference in temperature is within a degree of accuracy that is reliable. But there is more to the calibration on these instruments than there is for a thermometer. With an IR thermometer, there is a single focal point that senses the temperature of the skin. During calibration, a thermometer is checked at multiple temperature values across its designed measuring range to ensure it is maintaining its accuracy no matter what temperature you are reading. The same holds true for a thermal imager or line scanner with regard to checking multiple temperature values across the measuring range (see fig. 2). But, with these devices pixel calibration across the image is just as important. Again, a thermometer has a single focal point for temperature measurement while a thermal imager (which is a camera that uses the infrared spectrum) measures multiple points at once across the image.
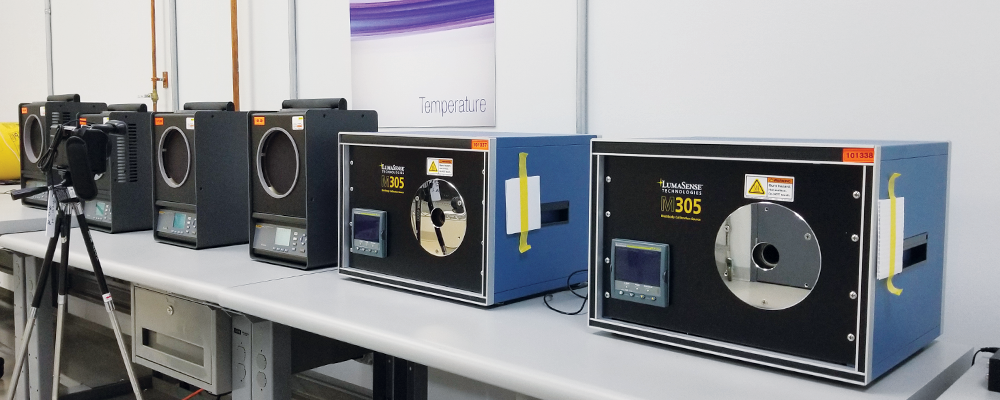
Figure 2: Calibration of a Thermal Imager Using Blackbody Sources
It is important to know how much the temperature varies across the entire image (known as uniformity) as well as how that changes at different temperature values across the imager’s measuring range. So, the calibration of an imager/scanner needs to check the error of the pixels in the upper right region of the image as well as the pixels in the lower left, center, etc. With a thermal imager that is 1280 pixels wide x 960 pixels high, that is 1.2 million pixels that could have different temperature results! Not to worry, not all 1.2 million pixels need to be checked individually. Because the image being monitored covers a region of thousands of pixels, it is only necessary to check the imager in multiple regions across the screen – repeated at multiple temperatures across the measuring range. Usually a 5-point or 9-point Uniformity test is included or can be added to the calibration (see fig. 3).
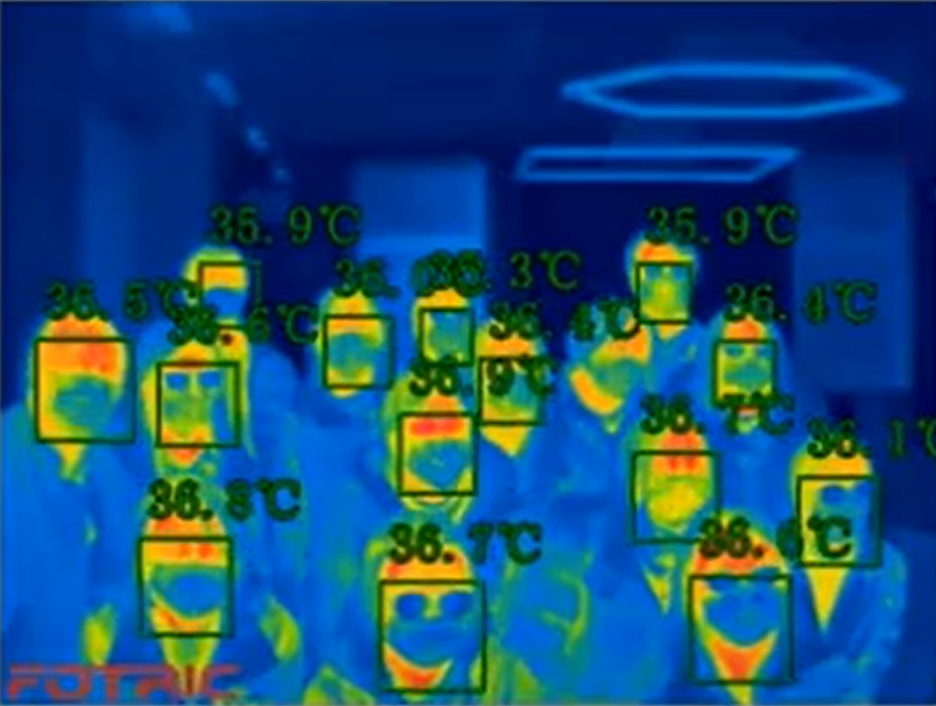
Figure 3: Locations of a 9-point Uniformity test in the calibration of a thermal imager/line scanner.
Conclusion
The post-COVID world has changed how we must live in society and operate our businesses. Fortunately, technology allows us to continue to live and work, whether interacting remotely through video conferencing or intermingling using social distancing, hand-washing, and masks to stay safe. Self-monitoring and social-monitoring for Elevated Body Temperature (EBT) are an important part of preventing the spread of infectious disease. Social-monitoring can be accomplished for small volumes using non-contact thermometers and contact traceability lists. For large volume monitoring, thermal imagers and line scanners are more efficient as a ‘hot spot’ check followed by non-contact thermometer use for suspected febrile individuals, also using a contact traceability list. If those individuals are confirmed to have a fever at or above 100.4 °F, they can then seek medical advice for further evaluation and possible COVID-19 testing. This filtered approach to discovering higher risk individuals is becoming the new normal for society. If you should have questions about the right instruments to use for accurate EBT monitoring or about calibration of your instruments, contact a trusted professional at Transcat: 1-800-633-0561 or transcat.com.
